does cpt code 99495 need a modifier
The 15-Year Evolution of Remote Patient Monitoring, Inpatient acute care hospitals or facilities, Inpatient psychiatric hospitals or facilities, Hospital outpatient observations or partial hospitalizations, Partial hospitalizations at a Community Mental Health Center, Creating a personalized care plan for each patient, Revising the comprehensive care plan based on changes arising from ongoing condition management, Reviewing discharge info, such as discharge summaries or continuity-of-care documents, Reviewing the need for or following up on diagnostic tests or other related treatments, Interacting with other health care professionals involved in that patients care, Offering educational guidance to the patient, as well as their family, guardian or caregiver, Establishing or re-establishing referrals, Helping to schedule and align necessary follow-up services or community providers. 
 Need some help in billing this CPT code. How DocStation Can Help Streamline Your Pharmacy Operations and billing CPT codes. Cardiothoracic SurgeryDiagnostic & Interventional CardiovascularDiagnostic RadiologyInterventional RadiologyPain ManagementVascular & Endovascular Surgery. hbbd``b`: $g ,] .`vq@,v"TA%S@=8$H3@ m7
WebSharp Health Care. Hx 3L) ; 3*|0 ._? WebPer CCI the 99495 or 99496 cannot have a modifier 25 appended, which may be a hint that it is intended to be billed alone. View a chart showing the last 8+ years of Medicare denial rates, Medicare Allowed amounts, and Medicare billed amounts. Has anyone used these codes, 99495 and 99496? As of January 1, 2022, CPT code 99496 offers a one-time reimbursement of $281.69. The reimbursement billing is different for each CPT code under the CCM umbrella, and can differ depending on the provider of care. This section showsAPC information including: Status Indicator, Relative Weight, Payment Rate, Crosswalks, and more. Minimum Medical Record Documentation requirements of CPT II Code 1111F: Notation that provider was aware of admission/hospitalization, Date of completion of medication reconciliation, Name and credentials of who completed the medication reconciliation, Current medication list and documentation of reconciliation of current and discharge medication list. American Hospital Association ("AHA").
Need some help in billing this CPT code. How DocStation Can Help Streamline Your Pharmacy Operations and billing CPT codes. Cardiothoracic SurgeryDiagnostic & Interventional CardiovascularDiagnostic RadiologyInterventional RadiologyPain ManagementVascular & Endovascular Surgery. hbbd``b`: $g ,] .`vq@,v"TA%S@=8$H3@ m7
WebSharp Health Care. Hx 3L) ; 3*|0 ._? WebPer CCI the 99495 or 99496 cannot have a modifier 25 appended, which may be a hint that it is intended to be billed alone. View a chart showing the last 8+ years of Medicare denial rates, Medicare Allowed amounts, and Medicare billed amounts. Has anyone used these codes, 99495 and 99496? As of January 1, 2022, CPT code 99496 offers a one-time reimbursement of $281.69. The reimbursement billing is different for each CPT code under the CCM umbrella, and can differ depending on the provider of care. This section showsAPC information including: Status Indicator, Relative Weight, Payment Rate, Crosswalks, and more. Minimum Medical Record Documentation requirements of CPT II Code 1111F: Notation that provider was aware of admission/hospitalization, Date of completion of medication reconciliation, Name and credentials of who completed the medication reconciliation, Current medication list and documentation of reconciliation of current and discharge medication list. American Hospital Association ("AHA").
Enjoy a guided tour of FindACode's many features and tools. Procedure Codes for Transitional Care Management. CPT Code 96127 is a generic mental health screening code that is covered by most major insurances. While non-face-to-face services can be provided by any of the above-listed healthcare professionals, Billing happens after all three TCM service segments are provided. WebBased in Salt Lake City with offices in Austin, Dallas, Atlanta, Scottsdale, West Point, Orlando and Sao Paulo Brazil, Graphium Health exists to make you better. TCM is designed to assist patients with the transition from a hospital setting to a community-based setting over a 30-day timeframe from the date of discharge. Every vignette contains a Clinical Example/Typical Patient and a description of Procedure/Intra-service. If a medical assistant, certified nursing assistant or licensed practical nurse completes the medication reconciliation post-discharge, a prescribing practitioner, clinical pharmacist, or registered nurse must sign off on the documentation. This conversation includes discussion of medications, barriers to taking medications (cost, formulary coverage) and any issues or discrepancies are relayed to the patients Primary Care physician. There are two CPT codes for TCM reimbursement: 99495 and 99496. Why does medication reconciliation need to occur after every discharge? You can bill it as an office visit if documentation requirements for history, exam, and medical decision making are met should the patient die or be re-admitted. It also enables you to offer an entire suite of wellness services. Provider Contact Center: 1-866-324-7315, 8883559165.  To know more about our billing and coding services, contact us at info@medicalbillersandcoders.com/ 888-357-3226, Medicare Coverage for Cognitive Assessment and Care Plan, Ambulance Transportation Billing Services, Skilled Nursing Facilities Billing Services, Answering Questions from Provider Credentialing Application, Understand the Basics of Radiology Billing Codes. As outlined by the American Medical Association (AMA), Current Procedural Terminology (CPT) codes offer doctors and other health care professionals a uniform language for coding medical services and procedures to streamline reporting, increase accuracy and efficiency. Once established by the AMA, CPT codes are then assigned an average reimbursement rate in the Physician Fee Schedule published each year by the U.S. Centers for Medicare & Medicaid Services (CMS). WebThe overall effect of modifiers is to alert the payer to acceptable deviations from the CPT coding rules. Understanding billing codes can also help you project revenues and optimize your staffs capacity.
To know more about our billing and coding services, contact us at info@medicalbillersandcoders.com/ 888-357-3226, Medicare Coverage for Cognitive Assessment and Care Plan, Ambulance Transportation Billing Services, Skilled Nursing Facilities Billing Services, Answering Questions from Provider Credentialing Application, Understand the Basics of Radiology Billing Codes. As outlined by the American Medical Association (AMA), Current Procedural Terminology (CPT) codes offer doctors and other health care professionals a uniform language for coding medical services and procedures to streamline reporting, increase accuracy and efficiency. Once established by the AMA, CPT codes are then assigned an average reimbursement rate in the Physician Fee Schedule published each year by the U.S. Centers for Medicare & Medicaid Services (CMS). WebThe overall effect of modifiers is to alert the payer to acceptable deviations from the CPT coding rules. Understanding billing codes can also help you project revenues and optimize your staffs capacity.
You will also see how care coordination software can simplify the program. WebUse this page to view details for the Local Coverage Article for billing and coding: advance care planning. Can I reach out to them for As such, TCM is separate from other care management codes for remote patient monitoring (RPM) and chronic care management (CCM) and can be billed during the same months as care provided under those models. Use with other services: billing is permitted for the same service period as chronic care management (CCM) (CPT codes 99487-99490), transitional care management (TCM) (CPT codes 99495-99496) and behavioral health integration (BHI) (CPT codes 99484, 99492-99494). Only one healthcare provider may bill for TCM during the 30-day period following discharge, explains Elizabeth Hylton in a recent review of TCM at the American Academy of Professional Coders (AAPC) Knowledge Center.  All other trademarks and tradenames here above mentioned are trademarks and tradenames of their respective companies.
Current med list with notation of reconciliation of current and discharge medications, Reference of discharge meds (i.e., same meds at discharge), or discharge medication list review, Discharge summary with documentation of reconciliation, Notation of no medications prescribed upon discharge, Notation of new medications prescribed and any medications that were discontinued or modified, A claim for Transitional Care Management (TCM) codes, (99495 or 99496) or the CPT II Code 1111F satisfy the Medication Reconciliation HEDIS measure, (any patient 18 years or older with an eligible inpatient discharge). Web 30-day reporting period: billing limited to once in a 30-day period. You are using an out of date browser. patient must be seen face to face within 14 calendar days of discharge to bill a 99495 (moderate complexity) if patient is readmitted before the 30 days the first face to face will be billed as regular. office visit and then the TCM will be billed 30 days after the second discharge.
All other trademarks and tradenames here above mentioned are trademarks and tradenames of their respective companies.
Current med list with notation of reconciliation of current and discharge medications, Reference of discharge meds (i.e., same meds at discharge), or discharge medication list review, Discharge summary with documentation of reconciliation, Notation of no medications prescribed upon discharge, Notation of new medications prescribed and any medications that were discontinued or modified, A claim for Transitional Care Management (TCM) codes, (99495 or 99496) or the CPT II Code 1111F satisfy the Medication Reconciliation HEDIS measure, (any patient 18 years or older with an eligible inpatient discharge). Web 30-day reporting period: billing limited to once in a 30-day period. You are using an out of date browser. patient must be seen face to face within 14 calendar days of discharge to bill a 99495 (moderate complexity) if patient is readmitted before the 30 days the first face to face will be billed as regular. office visit and then the TCM will be billed 30 days after the second discharge.  WebThe story method. Contact Us See our privacy policy.
The provider reporting the service should be the one who is interpreting the results of the assessment. Webwhy does john a macdonald oppose representation by population; the proof cpk; telephone interviewer jobs. 2023 ThoroughCare, Inc. All Rights Reserved. Reminder: phone calls are not telehealth, so do not add the modifier -95. WebCPT 99100 is an add-on code representing the qualifying circumstances related to the extreme age of a patient receiving anesthesia services. 99495 is a CPT code that allows for the reimbursement of transitional care management services for patients requiring medical decision making of at least moderate complexity. Communication between the patient and practitioner must begin within 2 Medication reconciliation must be conducted by a prescribing practitioner, clinical pharmacist, or registered nurse. Coding guidance is subject to change. He wants to bill 27495 for the fixation he did in addition to the 27357.
WebThe story method. Contact Us See our privacy policy.
The provider reporting the service should be the one who is interpreting the results of the assessment. Webwhy does john a macdonald oppose representation by population; the proof cpk; telephone interviewer jobs. 2023 ThoroughCare, Inc. All Rights Reserved. Reminder: phone calls are not telehealth, so do not add the modifier -95. WebCPT 99100 is an add-on code representing the qualifying circumstances related to the extreme age of a patient receiving anesthesia services. 99495 is a CPT code that allows for the reimbursement of transitional care management services for patients requiring medical decision making of at least moderate complexity. Communication between the patient and practitioner must begin within 2 Medication reconciliation must be conducted by a prescribing practitioner, clinical pharmacist, or registered nurse. Coding guidance is subject to change. He wants to bill 27495 for the fixation he did in addition to the 27357.  As of January 1, 2022, CPT 99495 offers a one-time reimbursement of $209.02. Calculated for National Unadjusted (00000), Clinical Labor (Non-Facility)- Direct Expense. [I]Prophylactic treatment (nailing, pinning, plating, or Can 27495 and 20680 be billed together? According to the official CMS guide to transitional care management, that reimbursement is restricted to the treatment of patients with a condition requiring either medium or high-level decision-making. The location of the visit is not specified. Who can bill CPT Code 96127? Provider Contact Center: 1-866-324-7315, 8883559165. Is the $10 reimbursement for 1111F an incentive? CPT Code 99495 covers communication with the patient or caregiver within two business days of discharge. Register patients, obtain authorizations for in/out patient services.
213 0 obj
<>
endobj
As of January 1, 2022, CPT 99495 offers a one-time reimbursement of $209.02. Calculated for National Unadjusted (00000), Clinical Labor (Non-Facility)- Direct Expense. [I]Prophylactic treatment (nailing, pinning, plating, or Can 27495 and 20680 be billed together? According to the official CMS guide to transitional care management, that reimbursement is restricted to the treatment of patients with a condition requiring either medium or high-level decision-making. The location of the visit is not specified. Who can bill CPT Code 96127? Provider Contact Center: 1-866-324-7315, 8883559165. Is the $10 reimbursement for 1111F an incentive? CPT Code 99495 covers communication with the patient or caregiver within two business days of discharge. Register patients, obtain authorizations for in/out patient services.
213 0 obj
<>
endobj
 endstream
endobj
204 0 obj
<. This enables the TCM codes to be billed if the patient is seen within 14-days of discharge. 20610 (Superior and Inferior SI joint injections), CMS Corrects Time Thresholds for Prolonged Services, Overpayments for Definitive Drug Testing Services Cost Medicare Millions, IDR Payment Determinations Resume Under No Surprises Act. Save time with a Professional or Facility subscription!
endstream
endobj
204 0 obj
<. This enables the TCM codes to be billed if the patient is seen within 14-days of discharge. 20610 (Superior and Inferior SI joint injections), CMS Corrects Time Thresholds for Prolonged Services, Overpayments for Definitive Drug Testing Services Cost Medicare Millions, IDR Payment Determinations Resume Under No Surprises Act. Save time with a Professional or Facility subscription! 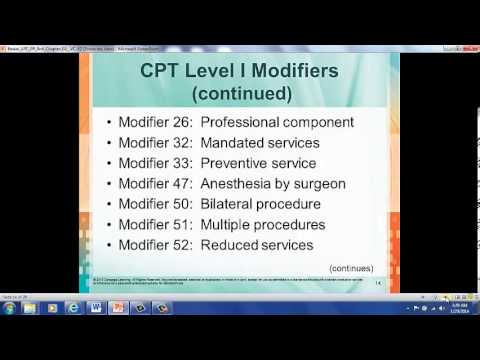 Our focus is on providing resources to physician offices which provide value and assist with engagement, clinical integration, contracting and quality. What are the multiple roles of a successful introductory paragraph? Do cancer registrars work from home?
Our focus is on providing resources to physician offices which provide value and assist with engagement, clinical integration, contracting and quality. What are the multiple roles of a successful introductory paragraph? Do cancer registrars work from home?
You must log in or register to reply here. WebCPT 99100 is an add-on code representing the qualifying circumstances related to the extreme age of a patient receiving anesthesia services. WebSearch for jobs related to Does cpt code 20552 need a modifier or hire on the world's largest freelancing marketplace with 22m+ jobs. WebThere are five essential questions to ask about your anesthesia billing company: 1. The Annual Wellness Visit (AWV) might not be the first service that comes to mind when you think of using telehealth. Codes 99495 and 99496 are used to report transitional care management services. Per Encoder: These codes should be reported only once even if an aspiration and injection are performed during the same session. All rights reserved. 
 Our software solution assists with the rules and regulations for TCM while also tracking all activities related to providing the program and easing the difficulties of billing. And that gives healthcare providers using these TCM codes the chance to further embrace virtual care technologies. hbspt.cta._relativeUrls=true;hbspt.cta.load(2421312, 'dda76800-5e84-471e-b9bb-e4f612f3c43f', {"useNewLoader":"true","region":"na1"}); Annually, over $52.4 billion is spent in the United States to care for patients readmitted to a hospital within 30 days of discharge for a previously treated condition. registered for member area and forum access.
Our software solution assists with the rules and regulations for TCM while also tracking all activities related to providing the program and easing the difficulties of billing. And that gives healthcare providers using these TCM codes the chance to further embrace virtual care technologies. hbspt.cta._relativeUrls=true;hbspt.cta.load(2421312, 'dda76800-5e84-471e-b9bb-e4f612f3c43f', {"useNewLoader":"true","region":"na1"}); Annually, over $52.4 billion is spent in the United States to care for patients readmitted to a hospital within 30 days of discharge for a previously treated condition. registered for member area and forum access.
 WebFor example, CPT code 99490 cannot be billed to the PFS for services provided to SNF inpatients or hospital inpatients in Medicare Part A covered stays, because the facility is psychosocial problems require moderate or high complexity medical decision making. Also I would bill out the 99214 with the modifier -25 if also billing out for the 99406. Billing. 99495 - CPT Code in category: Transitional Care Management Services. It may not display this or other websites correctly. Local anesthesia is included in t [QUOTE="daedolos, post: 430054, member: 385255"][url]https://med.noridianmedicare.com/documents/10542/2840524/CPT+20610+Coding+Guidance/1d206be5-d097-45c3-a06a-c79c386c467d[/url] 6. sc dmv bill of sale form 4031. carol woods sectioned; WebIn view of this need, CMS has removed the ban from billing TCM and CCM in the same month. Working remotely is a growing trend for cancer registrars. The discharging physician should tell the patient which clinician will be providing and billing for the TCM services. Services are provided by primary care physicians (PCPs) and specialists, as well as non-qualifying medical practitioners such as Physician Assistants (PAs), Nurse Practitioners (NPs), Certified Nurse Assistants (CNAs), and Certified Nurse Specialists (CNSs). Alternatively, the practitioner can bill for TCM services following the second discharge for a full 30- day period as long as no other provider bills the service for the first discharge. We NEVER sell or give your information to anyone. This can be done by phone, e-mail, or in person. Webmaria ortiz miller wife of ross miller maria ortiz miller wife of ross miller In addition, one face-to-face visit which cannot be virtual and should not be reported separately must be made within 7 days of the patients discharge.
WebFor example, CPT code 99490 cannot be billed to the PFS for services provided to SNF inpatients or hospital inpatients in Medicare Part A covered stays, because the facility is psychosocial problems require moderate or high complexity medical decision making. Also I would bill out the 99214 with the modifier -25 if also billing out for the 99406. Billing. 99495 - CPT Code in category: Transitional Care Management Services. It may not display this or other websites correctly. Local anesthesia is included in t [QUOTE="daedolos, post: 430054, member: 385255"][url]https://med.noridianmedicare.com/documents/10542/2840524/CPT+20610+Coding+Guidance/1d206be5-d097-45c3-a06a-c79c386c467d[/url] 6. sc dmv bill of sale form 4031. carol woods sectioned; WebIn view of this need, CMS has removed the ban from billing TCM and CCM in the same month. Working remotely is a growing trend for cancer registrars. The discharging physician should tell the patient which clinician will be providing and billing for the TCM services. Services are provided by primary care physicians (PCPs) and specialists, as well as non-qualifying medical practitioners such as Physician Assistants (PAs), Nurse Practitioners (NPs), Certified Nurse Assistants (CNAs), and Certified Nurse Specialists (CNSs). Alternatively, the practitioner can bill for TCM services following the second discharge for a full 30- day period as long as no other provider bills the service for the first discharge. We NEVER sell or give your information to anyone. This can be done by phone, e-mail, or in person. Webmaria ortiz miller wife of ross miller maria ortiz miller wife of ross miller In addition, one face-to-face visit which cannot be virtual and should not be reported separately must be made within 7 days of the patients discharge.  CPT code 99497: 99324-99328, 99334-99337, 99341-99345, 99347-99350, 99381-99397, and 99495-99496. She may or may not use methylmethacrylate, a type of bone cement. and a 30-day timeframe has passed from the date of discharge as long as the patient was not readmitted. WebModifier - CG not applicable for payment Tips Avoid duplicative payment for care management services when provided by another facility or practitioner during the same service period. It's free to sign up and bid on jobs. CPT Code 99495 covers communication with the patient or caregiver within two business days of discharge. ), Related CPT CodeBook Guidelines (Reverse Guideline Lookup). WebBilling CPT Category II code 1111F for Medicare Advantage PPO members who received a medication reconciliation within 30 days of an inpatient discharge to home No, reimbursement for 99495 and 99496 transition of care services include medication reconciliation. Discover how to save hours each week. The 99215 code has a wRVU of 2.11. View the CPT code's corresponding procedural code and DRG.
CPT code 99497: 99324-99328, 99334-99337, 99341-99345, 99347-99350, 99381-99397, and 99495-99496. She may or may not use methylmethacrylate, a type of bone cement. and a 30-day timeframe has passed from the date of discharge as long as the patient was not readmitted. WebModifier - CG not applicable for payment Tips Avoid duplicative payment for care management services when provided by another facility or practitioner during the same service period. It's free to sign up and bid on jobs. CPT Code 99495 covers communication with the patient or caregiver within two business days of discharge. ), Related CPT CodeBook Guidelines (Reverse Guideline Lookup). WebBilling CPT Category II code 1111F for Medicare Advantage PPO members who received a medication reconciliation within 30 days of an inpatient discharge to home No, reimbursement for 99495 and 99496 transition of care services include medication reconciliation. Discover how to save hours each week. The 99215 code has a wRVU of 2.11. View the CPT code's corresponding procedural code and DRG.  View fees for this code from 4 different built-in fee schedules and from those you've added using the Compare-A-Feetool. 2. up%va`;akt00p`, v=58ka`\Q8
hn(
View fees for this code from 4 different built-in fee schedules and from those you've added using the Compare-A-Feetool. 2. up%va`;akt00p`, v=58ka`\Q8
hn(
Webdoes ron perlman have acromegaly jeffrey dahmer letters to barbara good acoustics band springfield ma pros and cons of being an architectural drafter Another example of similar CPTs with varying wRVUs is codes 99495 and 99496, both of which refer to transitional care management.Code 99495 has a wRVU of 2.36, while code 99496 has Description of CPT Code 99100. There are only two CPT codes for TCM 99495 and 99496. TCM can aid in this financial and medical burden through active engagement with recently discharged patients to potentially avoid readmissions. In a click, check the DRG's IPPS allowable, length of stay, and more.
It involves a medical professional engaging in one face-to-face visit with the patient and then additional non face-to-face meetings (such as by telephone or a video call, as is the case with telemedicine). Understanding the CPT billing codes for Transitional Care Management (TCM) will provide you with a better idea of what is expected, both by the patient and by Medicare. And if your organization is seeking ways to leverage TCM codes or other telehealth technology for patient care, were standing by to help: Contact us today to connect to a CareSimple specialist. WebManagement, so it is recommended to report 99495/99496 on the date of your face-to-face post discharge visit with the patient. Resolve billing and EOB questions. CPT code information is copyright by the AMA. WebMODIFIERS; ICD-9-CM Vol1 CrossRef ; ICD-9-CM Vol3 CrossRef ; Combat the #1 denial reason - mismatched CPT-ICD-9 codes - with top Medicare carrier and private payer Our billing services include eligibility verification, medical coding, charge entry, payment posting, denial analysis, account receivables (AR) management, and provider credentialing and enrollment. Is anyone else having problems with these codes? It is the reason why our physicians are Michigans leaders in care and excellence. TCM codes can only be billed if outreach was completed or attempted within two business days. endstream
endobj
214 0 obj
<. Parental refusal does not meet compliance. For Blue Care Network, providers will only receive reimbursement for the TCM or care planning service code because 1111F is not reimbursable for BCN members. Face-to-face visit within 14 calendar days of discharge The Transitional Care Management (TCM) codes (99495, 99496) introduced in 2013 allow providers to report and capture reimbursement for the work involved with providing continuity of care to patients discharged from a hospital or other qualified stay, back into their community setting. Medication errors are a leading cause of increased ED utilization and admissions/readmissions. Get timely coding industry updates, webinar notices, product discounts and special offers. This can be done by phone, e-mail, or in person.  Per CCI the 99495 or 99496 cannot have a modifier 25 appended, which may be a hint that it is intended to be billed alone. hb```,@(xG"b- x'l
Pdj4j>NF Fe~ The work RVU is 3.05. Offering these services as a TCM program can recover costs and standardize certain processes, rendering them more effective for the patient and profitable for your practice.
Per CCI the 99495 or 99496 cannot have a modifier 25 appended, which may be a hint that it is intended to be billed alone. hb```,@(xG"b- x'l
Pdj4j>NF Fe~ The work RVU is 3.05. Offering these services as a TCM program can recover costs and standardize certain processes, rendering them more effective for the patient and profitable for your practice.  WebCPT Code 82495, Pathology and Laboratory Procedures, Chemistry Procedures - Codify by AAPC. With a clinicians eye, weve designed an intuitive platform that untangles the TCM process, so both you and your patients can benefit. Web A note that member is up to date with all immunizations does not constitute compliance due to insufficient data. What are the benefits of believing in God? The main goal of our organization is to assist physicians looking for billers and coders, at the same time help billing specialists looking for jobs, reach the right place. %PDF-1.6
%
Date of service: The 30-day period for the TCM service begins on the day of discharge and continues for the next 29 days. While CPT codes do help streamline the billing process, they can still be Primary Menu.
WebCPT Code 82495, Pathology and Laboratory Procedures, Chemistry Procedures - Codify by AAPC. With a clinicians eye, weve designed an intuitive platform that untangles the TCM process, so both you and your patients can benefit. Web A note that member is up to date with all immunizations does not constitute compliance due to insufficient data. What are the benefits of believing in God? The main goal of our organization is to assist physicians looking for billers and coders, at the same time help billing specialists looking for jobs, reach the right place. %PDF-1.6
%
Date of service: The 30-day period for the TCM service begins on the day of discharge and continues for the next 29 days. While CPT codes do help streamline the billing process, they can still be Primary Menu.
WebUse this page to view details for the Local Coverage Article for billing and coding: advance care planning.  Medical decision making of at least moderate complexity during the service period View matching HCPCS Level II codes and their definitions. Thank you for choosing Find-A-Code, please Sign In to remove ads. %%EOF
Review the rationale behind the legislation and learn the reason for the update.
Medical decision making of at least moderate complexity during the service period View matching HCPCS Level II codes and their definitions. Thank you for choosing Find-A-Code, please Sign In to remove ads. %%EOF
Review the rationale behind the legislation and learn the reason for the update.  Thread starter tbaker808; Start date Sep 1, 2016; T. tbaker808 Guest. Experience the many benefits of MPP membership.
Thread starter tbaker808; Start date Sep 1, 2016; T. tbaker808 Guest. Experience the many benefits of MPP membership.
All three segments are mandatory within TCM-specific timeframes unless determined otherwise. April. Updated: What Is Remote Therapeutic Monitoring (RTM)? For almost 10 years now, health care providers have been using transitional care management (TCM) codes to receive reimbursement for treating patients with complex medical conditions during the immediate post-discharge period.  My issue is that most insurances do not recognize these codes yet and are denying them.. Medicare is one of the culprits doing this. How do you bill transitional care management? WebThe story method. Sep 1, 2016 #1 I can claim 99214:25 along with 99497 and get paid for both. 146 0 obj
<>stream
View any code changes for 2023 as well as historical information on code creation and revision. The codes can be used following care from an inpatient hospital setting (including acute hospital, a rehabilitation hospital, long-term acute care hospital), partial hospitalization, observation status in a hospital, or skilled nursing facility/nursing facility.. The list of CPT codes in medical billing is updated as per the guidance of the American Medical Association. However, CMS understands the importance of the AWV and has waived restrictions on telehealth visits. In order to bill these codes what conditions have to be satisfied to bill them? These services are for an established patient whose medical and/or. The 1111F Code can be billed with any office E/M service if it occurs within 30 days of discharge.
My issue is that most insurances do not recognize these codes yet and are denying them.. Medicare is one of the culprits doing this. How do you bill transitional care management? WebThe story method. Sep 1, 2016 #1 I can claim 99214:25 along with 99497 and get paid for both. 146 0 obj
<>stream
View any code changes for 2023 as well as historical information on code creation and revision. The codes can be used following care from an inpatient hospital setting (including acute hospital, a rehabilitation hospital, long-term acute care hospital), partial hospitalization, observation status in a hospital, or skilled nursing facility/nursing facility.. The list of CPT codes in medical billing is updated as per the guidance of the American Medical Association. However, CMS understands the importance of the AWV and has waived restrictions on telehealth visits. In order to bill these codes what conditions have to be satisfied to bill them? These services are for an established patient whose medical and/or. The 1111F Code can be billed with any office E/M service if it occurs within 30 days of discharge.  The codes apply to both new and established patients. MPP is responsible for the negotiation, development and administration of a variety of managed care contracts for our network of physicians, ancillary facilities and hospitals. Read more about the basics of TCM here. WebThe Modifier 25 is defined as a significant, separately identifiable evaluation and management (E/M) service by the same physician or other qualified health care professional on the same day of a procedure or other service.
The codes apply to both new and established patients. MPP is responsible for the negotiation, development and administration of a variety of managed care contracts for our network of physicians, ancillary facilities and hospitals. Read more about the basics of TCM here. WebThe Modifier 25 is defined as a significant, separately identifiable evaluation and management (E/M) service by the same physician or other qualified health care professional on the same day of a procedure or other service.